As a new wave of NHS industrial action begins, a resident doctor has penned a stark account of the conditions driving her and her colleagues to strike in the middle of a severe winter flu crisis. Holly Tarn, who began working as a doctor just four months ago, describes a system buckling under the strain of 'super flu' cases, chronic staff burnout, and a bitter public relations battle with Health Secretary Wes Streeting.
A Hospital on Its Knees
The backdrop to the strike is a healthcare system under immense pressure. Influenza rates are currently double those seen at the same time last year, leading to emergency departments and wards being overwhelmed. In a bid to manage A&E overcrowding, patients who test positive for flu are often moved to respiratory wards, even when their primary medical issue is unrelated. This practice risks spreading the virus to some of the most vulnerable patients.
"Between 'super flu', fake news and fatigue, the hospital is on its knees," Tarn writes. She describes her own relentless workload, starting with a graphic encounter with a flu-positive, unvaccinated patient who will likely occupy a bed for days. The industrial action provides a difficult background hum, but for Tarn, the decision to strike is rooted in a fight for the profession's future.
The Personal Cost and Political 'Juvenile Delinquents'
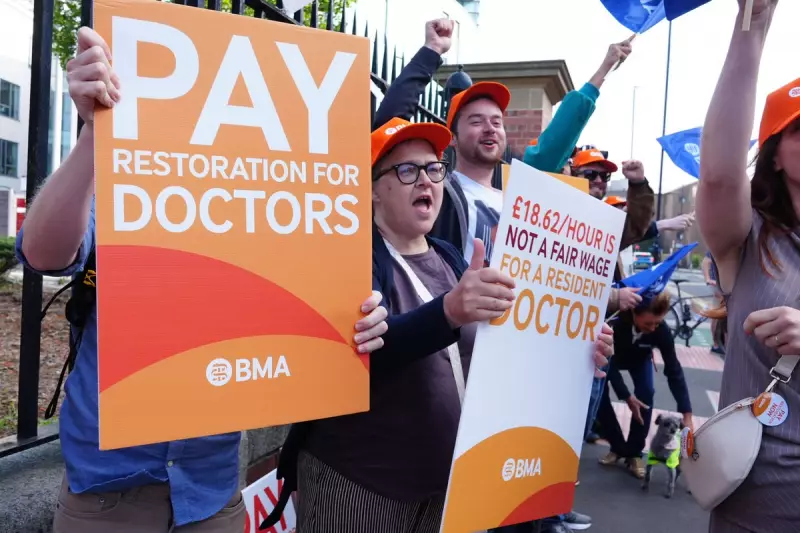
The article takes a personal turn as Tarn responds to recent comments from Health Secretary Wes Streeting, who labelled striking doctors as "moaning Minnies" and described the British Medical Association (BMA) as an organisation of "juvenile delinquency". For Tarn, a mother in her thirties with two young children, the remark felt deeply personal.
She outlines the sacrifices of her career: returning to medical school just six days after giving birth because students receive no maternity leave, accruing over £50,000 in debt, and now taking home around £2,000 a month after tax, almost half of which is spent on childcare. Her role as the resident doctor holding the medical 'bleep' overnight involves covering approximately 120 patients across six wards, a responsibility she argues makes the term "junior doctor" a serious misnomer.
Disputing the Government's Narrative
Tarn directly challenges the government's framing of the dispute, arguing the public is not hearing the full story. She disputes two key claims: on pay and on workforce planning.
While ministers cite a 28 per cent pay rise, Tarn states this ignores years of real-terms pay erosion and inflation. She characterises it as a starting point, not a settlement, noting next year's proposed increase would again fall below inflation.
On training posts, the government suggests a competition ratio of roughly two applicants per place. Tarn counters that for most entry-level specialty posts, the reality is closer to six applicants for every one position, with her own desired specialty seeing a ratio of 27 to one. She argues quoting an average obscures the intense bottlenecks early in a doctor's career.
Similarly, workforce plans for 4,000 new posts over three years are deemed insufficient against a shortfall Tarn estimates is closer to 20,000. The resident doctor concludes that the current offer does nothing to address the core issue of burnout. 83 per cent of doctors voted in favour of the strike action set to begin on Tuesday 16 December 2025.
Her final plea is to the public: "Please support your doctors. We want to serve the public. We just don’t want to drown in the process."





