Cambridge Research Reveals Menopause's Direct Impact on Brain Structure
A comprehensive new study from the University of Cambridge has established a significant connection between menopause and measurable changes in brain structure, potentially illuminating why women experience substantially higher rates of dementia compared to men. The groundbreaking research, published in the esteemed journal Psychological Medicine, examined data from an extensive cohort of 124,780 women to understand the neurological consequences of this pivotal life stage.
Grey Matter Reduction and Cognitive Implications
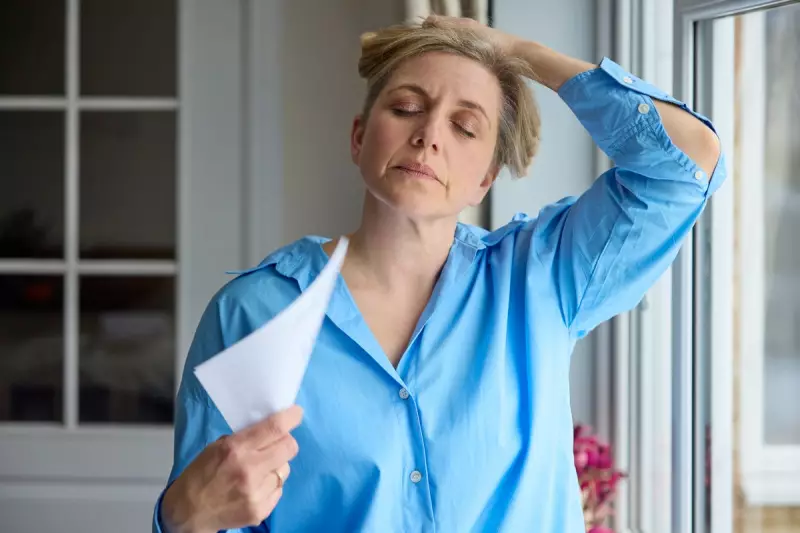
The investigation revealed that menopause is directly associated with a notable loss of grey matter – the vital brain tissue responsible for essential mental functions including memory, emotional regulation, and movement coordination. Beyond these structural alterations, the research documented how menopause can intensify existing issues such as anxiety, depression, and sleep disturbances, while also affecting recognised cognitive domains like thinking processes, attention span, language capabilities, and learning capacity.
Dr Katharina Zuhlsdorff from the University of Cambridge's psychology department explained the findings: "As we age, our reaction times naturally slow – this occurs in both women and men as part of the normal ageing process. However, menopause appears to accelerate this cognitive slowing significantly. While individuals might still reach correct answers in cognitive tasks, the processing speed diminishes noticeably."
Hormone Replacement Therapy's Protective Role
The study conducted detailed analysis regarding the potential protective effects of hormone replacement therapy (HRT). Researchers discovered that post-menopausal women who were not undergoing HRT treatment demonstrated markedly slower reaction times compared to both pre-menopausal women and those currently using HRT. Interestingly, the investigation found no substantial differences in memory task performance across these three distinct participant groups.
Dr Zuhlsdorff elaborated on HRT's apparent benefits: "Our findings suggest that while menopause accelerates cognitive ageing processes, hormone replacement therapy appears to apply the brakes, slowing this progression somewhat. This represents a significant insight for women navigating this transitional period."
Brain Region Vulnerability and Dementia Connection
Advanced magnetic resonance imaging (MRI) scans conducted on approximately 11,000 participants revealed significant reductions in grey matter volume specifically within brain regions known to be affected by Alzheimer's disease. These vulnerable areas included the hippocampus (crucial for learning and memory formation), the entorhinal cortex (essential for spatial navigation and memory consolidation), and the anterior cingulate cortex (responsible for attention regulation and emotional control).
Professor Barbara Sahakian, the study's senior author from Cambridge's psychiatry department, highlighted the implications: "The brain regions where we observed these structural differences are precisely those typically impacted by Alzheimer's disease. While not providing the complete explanation, this connection may help us understand why we see nearly twice as many dementia cases in women compared to men. Menopause could potentially render women more vulnerable to neurodegenerative conditions later in life."
Sleep Patterns, Fatigue, and Mental Health Considerations
The research documented that post-menopausal women were significantly more likely to report insomnia symptoms, obtain less overall sleep, and experience persistent tiredness compared to their pre-menopausal counterparts. Intriguingly, women undergoing HRT treatment reported the highest levels of fatigue among all three groups, despite sleeping similar amounts to post-menopausal women not receiving hormone therapy.
Dr Christelle Langley from Cambridge's psychiatry department noted: "Most women will experience menopause, representing a genuinely life-changing transition whether they opt for HRT or not. Maintaining a healthy lifestyle – incorporating regular exercise, sustained physical activity, and balanced nutrition – becomes particularly crucial during this period to help mitigate some of its more challenging effects."
Expert Perspectives and Practical Recommendations
Michelle Dyson, chief executive of the Alzheimer's Society, contextualised the findings: "Women constitute approximately two-thirds of individuals living with Alzheimer's disease in the United Kingdom. While we haven't yet fully comprehended why they demonstrate greater susceptibility than men, hormonal factors are increasingly considered significant contributors. This substantial study adds to mounting evidence demonstrating how menopause impacts brain structure, including physical changes like volume reduction."
Dr Louise Newson, a general practitioner and women's hormone specialist, emphasised the clinical importance: "Numerous women report noticeable changes in memory and concentration around menopause, and this research suggests these symptoms possess genuine biological foundations rather than simply representing normal ageing or stress responses. This highlights menopause as a critical period for brain health where timely, individualised medical care becomes particularly important."
The Alzheimer's Society recommends several evidence-based approaches for dementia risk reduction applicable to both women and men, including regular physical exercise, smoking cessation, and moderated alcohol consumption. For individuals concerned about themselves or family members, the organisation provides a dementia symptoms checklist as a practical first step toward initiating conversations with healthcare professionals.





