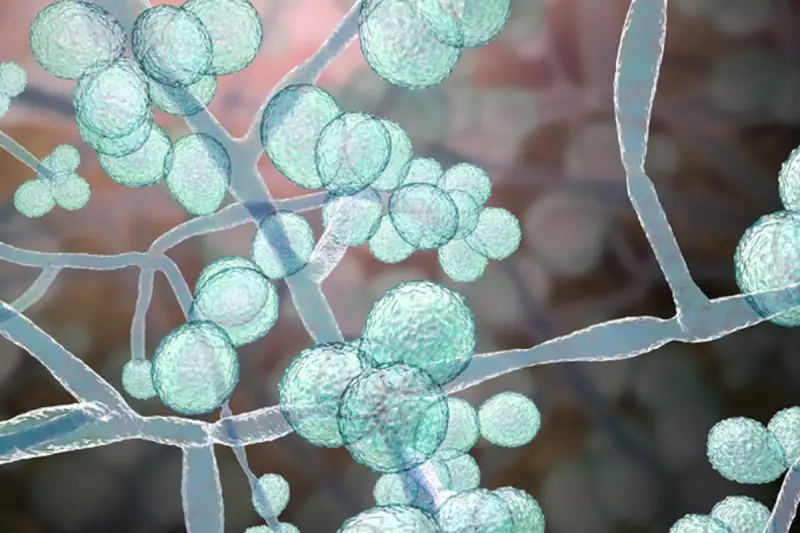
A dangerous and highly drug-resistant fungus is spreading across the United States at an alarming rate, posing a severe threat to vulnerable patients in hospitals and care homes, according to the latest health warnings.
What is Candida Auris and Why is it So Dangerous?
Health officials from the Centers for Disease Control and Prevention (CDC) report that Candida auris has now infected at least 7,000 people across 27 U.S. states. This invasive yeast is particularly lethal for individuals with weakened immune systems. The situation is escalating rapidly, with current 2025 case numbers fast approaching last year's record of over 7,500 infections.
"If you get infected with this pathogen that's resistant to any treatment, there's no treatment we can give you to help combat it. You're all on your own," explained Melissa Nolan, an assistant professor of epidemiology at the University of South Carolina, in an interview with Nexstar. The fungus's resistance to all major classes of antifungal drugs earns it the ominous label of a 'superbug'.
How the Fungus Spreads and Evades Treatment
The CDC states the fungus spreads easily in healthcare environments. A significant concern is its ability to survive on surfaces like bed rails and equipment. "It's really good at just being, generally speaking, in the environment," Professor Nolan said, noting that any pathogens missed during cleaning can become resistant and proliferate.
Compounding the problem, Candida auris is notoriously difficult to identify with standard laboratory tests, leading to dangerous delays in diagnosis and treatment. A recent scientific review highlighted its biological advantages: it can switch growth forms to spread, sticks to human skin "like glue," and forms protective layers. It also possesses "efflux pumps" that eject antifungal drugs before they can work.
A Growing Global Health Threat
This is not an isolated American crisis. The same study, published in Microbiology and Molecular Biology Reviews, notes that Candida auris has been identified in at least 61 countries across six continents. The fungus is gaining virulence and spreading rapidly on a global scale.
CDC epidemiologist Dr. Meghan Lyman emphasised the urgent need for action in a press release: "The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control."
Researchers are calling for the development of novel antifungal drugs, better diagnostic tools, and increased monitoring, especially in resource-poor nations. For now, the focus remains on stringent infection control in healthcare settings to protect the most at-risk populations from this relentless superbug.





