Residents of rural and coastal communities across England are set to benefit from improved access to cancer specialists under ambitious new government plans designed to dismantle what has been described as a 'postcode lottery' of care. The initiative forms the cornerstone of a comprehensive National Cancer Plan, scheduled for publication on World Cancer Day, February 4.
Targeting Workforce Shortages
The government has committed to creating additional training positions specifically within hospitals experiencing the most severe workforce shortages. These facilities are typically located outside major metropolitan centres, where consultant numbers are lower and patient waiting times are often significantly longer.
Health Secretary Wes Streeting, a kidney cancer survivor himself following treatment in London, emphasised the moral imperative behind the strategy. 'For too long, your chances of seeing a doctor and catching cancer early have depended on where you live,' he stated. 'That’s not fair and has to stop. I am determined to end the health inequalities that have grown across England over the last 15 years.'
Economic and Health Impacts
The plan recognises the profound link between healthcare access and local economic vitality. Areas with fewer oncology consultants and protracted diagnostic delays generally exhibit higher rates of economic inactivity. Treatment delays not only jeopardise health outcomes but also keep individuals out of the workforce, thereby restraining local economic growth.
'Faster diagnosis doesn’t just save lives – it gets people back to work and back to their families sooner,' Mr Streeting added, framing the policy as both a health and economic necessity.
Accelerating Technological Adoption
A key component of the forthcoming plan involves measures to rapidly deploy the latest diagnostic tests and medical technologies to hospitals nationwide. The goal is to ensure these innovations are not confined to traditional research-intensive sites, thereby democratising access to cutting-edge care.
From April 2027, a new system will be implemented whereby the National Institute for Health and Care Excellence (NICE) will assess novel tests and devices designed for earlier cancer detection. Once approved for NHS use, healthcare trusts will be mandated to offer them, mirroring the existing process for new medicines.
Pioneering Technologies Under Review
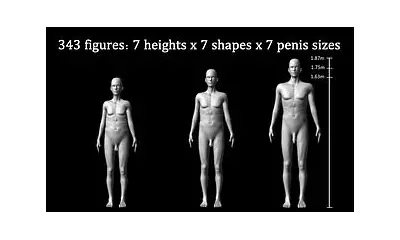
The first wave of technologies slated for NICE evaluation under this new model includes several promising innovations:
- Artificial intelligence systems capable of reading chest X-rays to aid in spotting lung cancer.
- Advanced software for analysing tissue samples to detect prostate and breast cancer.
- New techniques to provide faster answers for women experiencing unexplained vaginal bleeding.
- The 'sponge on a string' test for oesophageal cancer, which collects cells for analysis.
Professor Jonathan Benger, Chief Executive of NICE, commented: 'We’re now extending that same clarity and fairness to health tech. These reforms mean that clinically and cost-effective medical devices, diagnostics and digital tools will start to be reimbursed and made available consistently across the NHS.'
Addressing Stark Performance Gaps
The urgent need for reform is underscored by recent NHS England performance data. While 76.5% of patients urgently referred with suspected cancer in November received a diagnosis or had cancer ruled out within 28 days, this figure masked dramatic regional variation, ranging from 54.5% to 100% across different trusts.
A concerning disparity persists between the speed of ruling out cancer and confirming it. In November, 78.0% of patients were informed they did not have cancer within 28 days, but only 55.1% received a cancer confirmation within the same timeframe.
Broad Support for Action
Health charities and clinical leaders have welcomed the focus of the National Cancer Plan. Steven McIntosh of Macmillan Cancer Support noted, 'Right now, cancer care isn’t fair. Too many aren’t getting the treatment and care they need because of who they are and where they live.'
Professor Peter Johnson, National Clinical Director for Cancer at NHS England, affirmed that the plan would tackle differences in care 'head-on', aiming to ensure that whether a patient lives in a coastal town like Blackpool or a remote village, they receive an equitable standard of care and the same chance at survival.
The overarching mission, as articulated by the Health Secretary, is clear: 'Whether you live in a coastal town or a rural village, you deserve the same shot at survival and quality of life as everyone else. This government will turn that promise into a reality.'